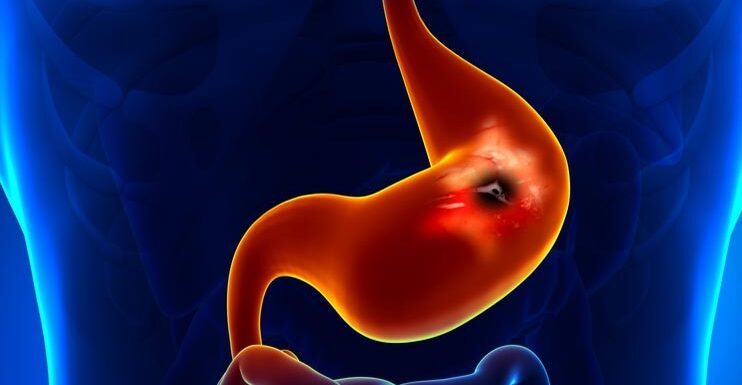
peptic ulcers
A peptic ulcer is a damaged area in the stomach or small intestine wall.
Your stomach makes acid to help you digest food. The stomach wall and the first part of your small intestine (duodenum) have a layer of mucus that protects them from acid.
If this protective mechanism doesn’t work correctly, the acid can eat away at your stomach lining and cause an ulcer.
Stomach (gastric) and small intestine (duodenal) ulcers are peptic ulcers. Duodenal ulcers are more common.
Stomach ulcers generally affect people between the ages of 40 and 80, and duodenal ulcers affect people between the ages of 20 and 60. Peptic ulcers are more common in women than in men.
Symptoms of peptic ulcers
However, many people have pain in the abdomen (belly), usually just below the chest bone (sternum). It usually only occurs after eating, 15 to 20 minutes later if you have a stomach ulcer, and one to three hours after a meal if the ulcer is in your small intestine.
Other symptoms may include:
- acidity
- Bitter taste in the mouth
- sickness or vomiting
- regurgitation of food
It is essential to see your GP if you:
- saw blood in your vomit or stool
- you have sudden and very severe abdominal pain
These symptoms may be caused by conditions other than a peptic ulcer. If you do, ask your GP for advice.
Complications of peptic ulcers
Most people who have a peptic ulcer do not have any complications. However, complications may include the following:
bleeding
Occasionally, ulcers can cause the lining of the stomach or small intestine to bleed. If this happens suddenly, it can include:
Vomiting blood may be bright red or coffee grounds (dark brown bits of coagulated blood)
Dark stools look black or tarry because the blood from the ulcer has partially broken down as it passes through the intestine.
Anaemia
If the ulcer bleeding is light, you may not see blood in your vomit or stool. However, you can develop anaemia. However, anaemia occurs when there are too few red blood cells or insufficient haemoglobin in the blood.
Drilling
Rarely, the ulcer may eat deep into the wall of your stomach or small intestine and make a hole in your abdomen. This is excruciating perforation, and you will need emergency surgery.
However, because drug treatment is usually successful, it is implausible that you will need surgery for a peptic ulcer.
Pyloric stenosis
Pyloric stenosis can occur if you have a peptic ulcer that causes long-term inflammation in the wall of your stomach or small intestine.
The narrowing of a small passage called the pylorus joins your stomach to the first part of your small intestine.
Causes of peptic ulcers
The most common cause is a stomach infection caused by Helicobacter pylori (H. pylori). This infection is quite common: nearly half of the world’s population is infected with the bacteria, but it does not always cause illness.
H. pylori can cause inflammation in the stomach wall. Inflammation occurs when part of the body reacts to an infection or injury by causing swelling, warmth, redness, and pain.
The inflammation reduces the mucus layer to protect the stomach and small intestine from stomach acids and causes an ulcer. If the H. Pylori infection occurs in the upper part of your stomach, it can increase acid production.
The second most common cause of ulcers is a class of nonsteroidal anti-inflammatory drugs- inflammatory drugs (NSAIDs).
Examples of these medications include aspirin, ibuprofen, naproxen, and diclofenac. Most people can take them safely, but sometimes taking NSAIDs for a long time can damage the mucus lining of your stomach and cause a peptic ulcer. If you doubt which pain relievers to handle, ask your pharmacist.
You are more likely to get peptic ulcers if you smoke.
It was thought that stress could cause a peptic ulcer, but stress is now only considered vital if it results from a major operation or trauma.
Diagnosis of peptic ulcers
Your GP will ask about your symptoms and examine you. He will also ask you questions about your medical history. For example, if your GP thinks you have a peptic ulcer, they may recommend one of the following tests to make a diagnosis and decide on the best treatment for you.
H.pylori test
Because H. pylori are the most common cause of a peptic ulcer, your GP can test you for the bacteria and, if necessary, prescribe medication to treat the infection. H. pylori can be detected on a urea breath test. You will have a breath test using a machine to measure the amount of carbon dioxide in your breath. If carbon dioxide exceeds a certain level, H. pylori are present.
endoscopy
If a peptic ulcer is suspected, your GP may schedule a gastrointestinal endoscopy (also called a gastroscopy). Unfortunately, not everyone with abdominal pain needs one, so your GP may use another test first. However, endoscopy is the only way to be sure whether or not you have a peptic ulcer.
An endoscopy is a procedure that allows a doctor to look inside your body. The test is done using a flexible tube-like telescopic camera called an endoscope passed through your mouth and stomach. The procedure usually takes a few minutes. Your doctor can see your stomach wall and take a sample simultaneously.
Treatment of peptic ulcers
self-help
You can make lifestyle changes to help your ulcers heal and prevent them from returning. These include: · not eating foods or drinks that cause more severe symptoms, such as spicy foods and alcohol · quitting smoking, · not taking pain relievers that are likely to cause ulcers in the future; your GP or pharmacist can give you advice on other medicines you can take instead.
Medicines
There are two main groups of medications available to treat peptic ulcers. They are the following:
- Proton pump inhibitors such as omeprazole and lansoprazole
- H2 blockers, examples include ranitidine and cimetidine.
Both types of medicine reduce the production of acids in the stomach, allowing your ulcer to heal. Both can be used long-term to prevent your ulcer from coming back. These medications will relieve your symptoms, and within a few weeks, your ulcer will heal. However, once you stop taking medicine, your ulcer may return unless the H. pylori have been treated and killed.
Treatment of an H. pylori infection
If the test confirms that you have H. pylori, you will be prescribed medication to treat it. This is usually a combination of a proton pump inhibitor and two antibiotics. Treating the H. pylori infection should help your ulcer heal and prevent it from returning. In addition, your GP will do other tests after treatment to ensure the H. pylori has been successfully eliminated.